About the project
Development of a national strategy for the care of seriously ill, dying and deceased adults and their relatives in times of pandemic. All areas of care that treat and support seriously ill and dying people have jointly developed recommendations for action and information material on palliative care for patients with/without infections.
This largest structured alliance of university palliative care centres in Germany to date has ensured that the needs of seriously ill and dying people and their relatives are effectively taken into account in the response to the pandemic, thereby improving treatment.
► more
The most important facts at a glance
The aim of the project is to develop and agree on a national strategy for the care of seriously ill, dying adults and their relatives in times of pandemic with
- Recommendations for general and specialised palliative care for patients with/without infection
- Collection and development of information material for an online information platform currently in preparation and
- Identification of variables for the scientific recording of palliative care in times of pandemic for the research database initiated by the National Research Network for University Medicine.
During the SARS-CoV-2 pandemic, medical care activities focussed primarily on setting up intensive care beds for acute COVID-19 patients. Despite the less severe course of the disease in Germany, over 115,000 people died from or with COVID-19 (as at January 2022). Reports and publications by those affected and (palliative) care providers made it clear that both the identification of individual patient preferences and the quality of care for the seriously ill and dying varied greatly.
The palliative medical care of seriously ill and dying people with and without an infectious event is the task of all healthcare professionals. This also applies in times of pandemic.
Specialised palliative care makes a significant contribution here, both directly in the care of those affected and indirectly by supporting primary care providers. Due to their expertise and experience, specialised palliative care providers, such as those in this network, are best placed to develop an appropriate national strategy for palliative care in times of pandemic in close cooperation with general care providers and specialists in hygiene, infectiology, infection medicine and others.
Structure of the palliative medicine research network
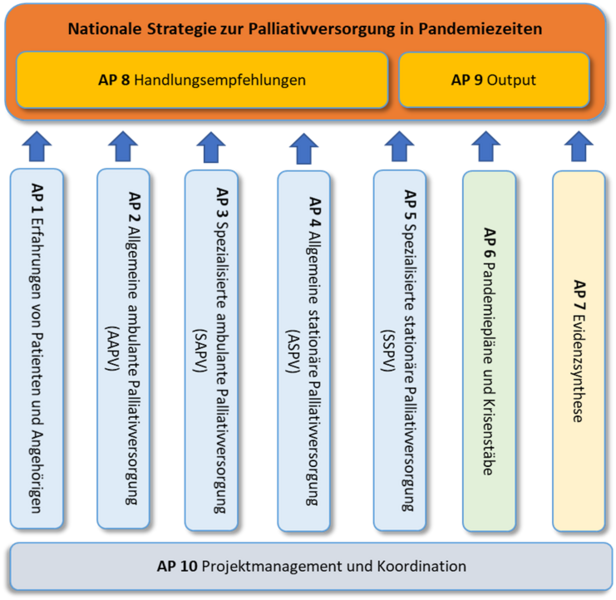
The palliative care research network analysed the current pandemic situation in 10 different work packages and developed the national strategy (see illustration).
Work packages 1-6 analysed the experiences from the current SARS-CoV-2 pandemic with regard to the (palliative) care of seriously ill and dying people and their relatives from the perspectives of patients and relatives (WP1), general and specialised palliative care in outpatient and inpatient settings (WP2-5) and the crisis teams at local, regional and national level (WP6). Particular care was taken to ensure that all areas of patient care that treat and support seriously ill and dying people were included and taken into account in the survey of their experience in the SARS-CoV-2 pandemic.
The national and international evidence on palliative care and the SARS-CoV-2 pandemic, or in pandemic situations in general, was researched and summarised in WP7. This work package also identified ongoing studies on palliative care during the SARS-CoV-2 pandemic, the results of which could be relevant for the national strategy and the recommendations for action.
The recommendations for action were developed from the beginning of the project in WP8. The results of the parallel WPs described above were continuously incorporated into the development of the recommendations for action.
Information materials and best practice examples were collected and analysed in WP 9 for the online information platform to be created.
WP 10 was used for project management and coordination of the research network.
All results of the work packages and the outputs (recommendations for action, material for the information platform and variables for the scientific survey) for the work packages described were made available to other projects in the Network University Medicine.
For future pandemic preparedness, national recommendations and concepts are needed to ensure that seriously ill and dying people receive high-quality end-of-life care even in a pandemic situation and that dignified dying is possible even in extreme situations. Relatives should be able to say goodbye to their loved ones in an appropriate manner even under difficult circumstances.
In addition, relevant information and training materials on palliative care in times of pandemic were collected and made available for the information platform planned by the NUM.
Highlights
In 16 studies, over 1,700 people affected, carers and those responsible in the healthcare system and in politics were asked about their experiences within 9 months and their statements were systematically analysed and evaluated. Based on these results and with the help of 120 experts from the various areas of healthcare, administration and politics, the National Strategy for the Care of the Seriously Ill and Dying and their Families in Times of Pandemic was then developed and agreed upon. At the heart of the strategy are 33 specific recommendations for action, which are divided into three sections: Supporting patients & relatives, supporting staff and supporting and maintaining palliative care structures and services. You can find all recommendations for action at the following link to the National Strategy for the Care of the Seriously Ill and Dying and their Families in Times of Pandemic (PallPan)
Following the publication of the recommendations for action, the PallPan consortium is already working on further projects: the development of a web-based information platform, the development of support materials for grieving relatives and employees in care facilities and hospitals, the integration of PallPan into a "National Pandemic Preparedness" for the German healthcare system and the continuous further development of the recommendations for action.
In addition, the PallPan consortium was honoured with the "DMW Walter Siegenthaler Prize" and third place in the German Patient Safety Award.